Rude comments, loud appearances or even threats — have you ever experienced that? Many practice teams report: The number of stressful situations is increasing.
According to the 2023 KBV survey, 75% of practices say that the number Aggressive patients have increased. Particularly affected: MFA at reception. They are the first point of contact — and often the first screen for dissatisfaction, anxiety or anger.
What used to be the exception is now becoming a stressful everyday life. The question is no longer whether It escalates — but when and How well prepared is the team.
Why do patient situations escalate?
The reasons are manifold — and rarely purely personal:
- Increased time pressure on both sides: Patients experience long waiting times, MFA struggles with time pressure and scarcity of resources.
- Frustration with the healthcare system: Lack of services, full waiting rooms, rejected treatments — many feel left alone.
- Anxiety & loss of control: People react emotionally, especially in exceptional health situations. Anxiety can result in anger or denial.
- Lack of communication skills: Patients have rarely learned how to communicate constructively. There may also be a lack of conversation techniques on the practical side.
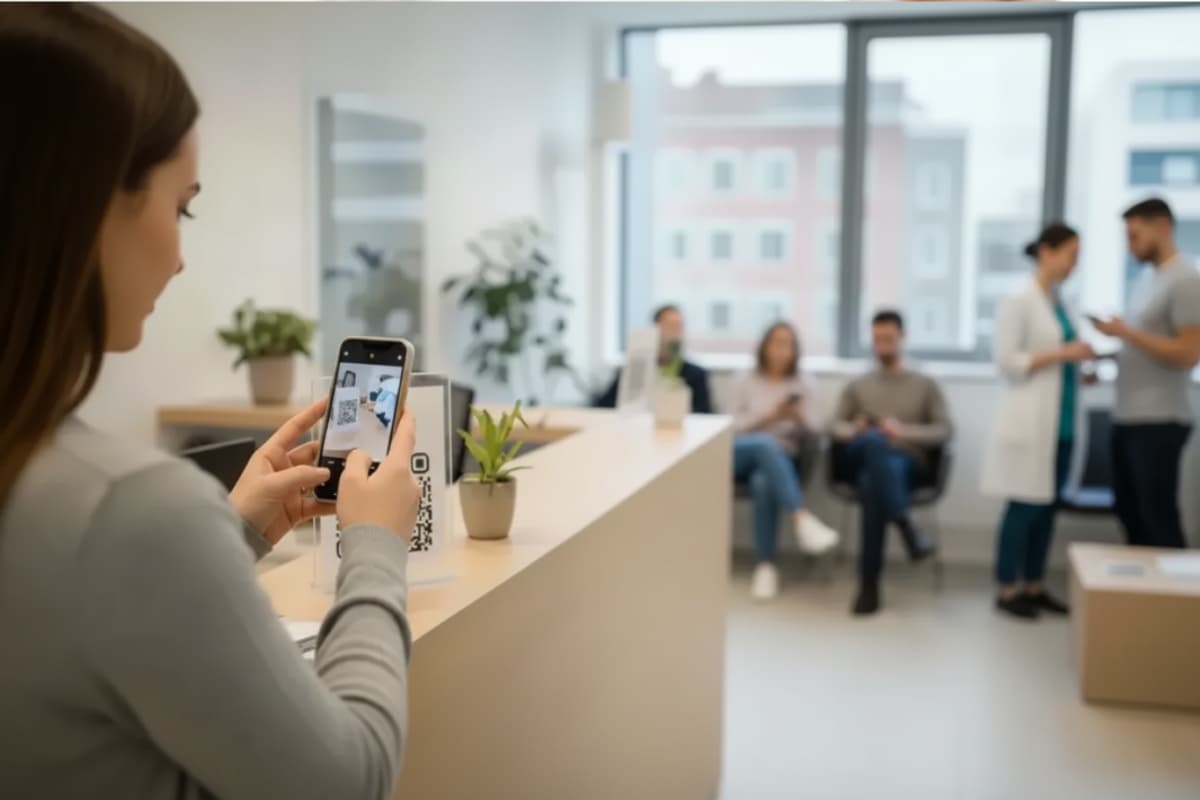
- Digitalization & new processes: Anyone who doesn't understand QR codes or apps feels excluded or overwhelmed.
What MFA can do specifically when dealing with difficult patients
Medical professionals are organizational talents and masters at multitasking, but not lightning rods. It is completely okay to set limits. Clear communication helps: Anyone who says early on what works and what doesn't protect themselves. For example: “I like talking to you, but only in a respectful tone.” Even simple stop sentences such as “I want you to keep your distance now” can provide security.
It is important to get support — bring in colleagues or supervisors when conflicts arise and hand over tasks when it gets too much. Incidents should be documented: Who was involved, what happened, when? Specific notes, such as telephone numbers or wording, help with threats.
It is also good to know where help is available: medical associations, professional associations such as vmf e.V., trade unions such as ver.di or BGW offer advice and training. Teams that strengthen each other experience less stress and more confidence in action, even in difficult moments.
Mitigate conflicts with de-escalation and self-confidence
Many conflicts can be alleviated if you remain calm. This can be trained: don't counter, take a deep breath, speak calmly and consciously take breaks. With clear body language and sentences such as “I see that you're angry”, you signal presence and willingness to talk.
Self-confidence grows through practice — for example in role-playing games, self-assertion training, or through voice and relaxation exercises. A clear stance helps to maintain limits without violating.
Psychological background: People reflect themselves unconsciously. Anyone who radiates peace is more likely to relax the other person — or intensify the conflict less.
Protection strategies and points of contact
Mental strength is important, but practice teams also need very specific protective mechanisms. This includes spatial security, such as privacy at reception, a distance between door and counter, or a de-escalation button. In critical situations, never enter into aggressive conversations alone. When in doubt, it is better to leave the room, bring in colleagues or address them specifically. An emergency checklist should be handy at all times.
Rules should be visible: For example, as a notice in the reception area or on the website. When incidents occur, documentation is mandatory: Who was involved, what happened? Practice management should be informed and — if necessary — reported. Psychological support is available through BGW or external specialists.
Teamwork and leadership: What strengthens practices from within
Dealing with difficult situations is not a task for MFA alone. Good leadership, clear structures and strong teamwork are crucial. Regular team meetings with space for specific cases help, as does practice management who sets a good example themselves.
Emergency plans should be set out in writing — who will do what if things get serious? Appreciation in everyday life, honest feedback and space for feelings strengthen cooperation. And very important: When practice owners visibly stand behind their team, it not only strengthens morale, but also sends patients a clear signal — rules apply here.
Conclusion: Strong together — even in storms
Difficult patient situations are no longer an exception today, but practice teams are not helplessly at the mercy of them. Good preparation, clear communication and genuine teamwork create security, even in tense moments.
Every practice can create safe spaces — spatially, emotionally and organizationally. The key lies in appreciation, clarity, and self-effectiveness.