How can patient communication be simplified with digital tools?
Digital tools simplify patient communication by Centralize information, automate processes, and avoid errors. When recurring processes are digitized, everyone involved benefits: The practice works more efficiently, patients feel better informed — and the personal conversation regains space for the essentials. Learn six particularly effective levers for easier patient communication.
1. Digital anamnesis: less paper, more precision
Patients fill out their medical history forms conveniently online — at home or on their smartphone before the appointment. This means that all relevant information is already available when treatment starts. Die digital anamnesis with Nelly saves time at reception, reduces inquiries and reduces the risk of transmission errors. At the same time, healthcare professionals can address complaints or pre-existing conditions in a more targeted manner because all data is available in a complete and structured manner.
2. Digital signature: sign faster and legally secure
Consent declarations, clarification forms or data protection forms can easily be digitally signed with Nelly. that Facilitates the digital document transfer, saves printing costs and paper and meets all data protection and legal security requirements.
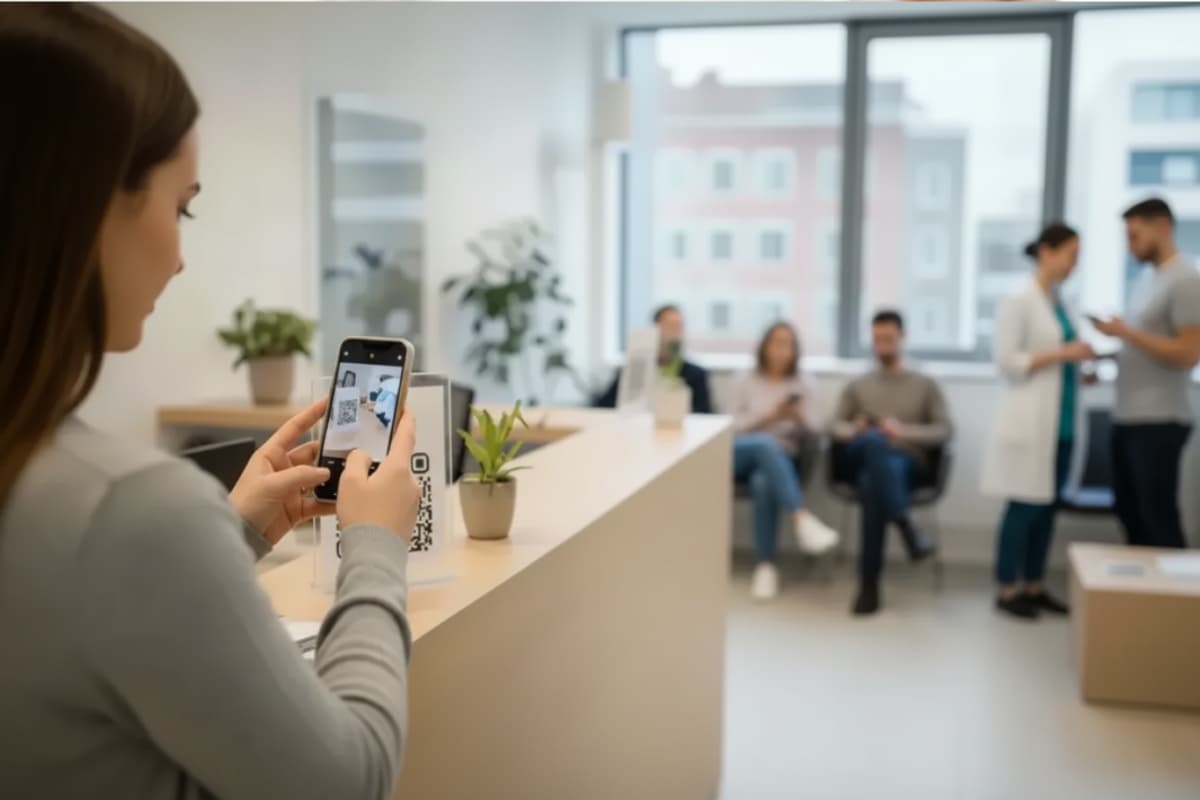
3. Patient portal: central interface for exchange and service
The modern Patient portal by Nelly bundles communication, documents and invoices in one place. Patients can access all their documents at any time and can also conveniently pay bills on their own smartphones, e.g. via Apple Pay.
The practice team also benefits: Recalls and inquiries are becoming fewer, processes are becoming more transparent and accessibility is significantly improving.
4. Telemedicine: digital consultation
Telemedicine with platforms such as TeleClinic enables medical care regardless of time and place — via video, telephone or digital exchange of findings. It makes practice processes more efficient, reduces waiting times and relieves the entire team. Routine or aftercare appointments can be conveniently held online, while more complex cases are dealt with specifically in practice.
As a result, the number of patients on site is better managed: The waiting room stays more relaxed Processes are more structured and medical staff can spend more time with patients who are actually on site. Telehealth also offers great benefits for chronically ill or immobile people — they stay in close contact with their doctor without having to go long distances or long waiting times.
5. Remote patient monitoring: Remote Patient Controling (RPM)
Remote patient monitoring continuously records health data such as heart rate, blood pressure or blood sugar — both with dedicated medical devices and with simple smartwatches or fitness gadgets. This is how the doctor receives reliable values from everyday life of the patient, not just snapshots during a practice visit.
Especially in the case of chronic diseases or cardiovascular problems, changes can be identified at an early stage and treatments can be specifically adapted. Many symptoms, which are often no longer measurable in practice, become visible and comprehensible through RPM.
In practice, this means: better basis for decision-making, fewer emergencies and closer patient loyalty. At the same time, patients feel safer because they know that their values are regularly checked — without having to stop by in person all the time.
How does GDPR-compliant patient communication work?
Patient communication is subject to particularly high data protection requirements. According to the General Data Protection Regulation (GDPR), health data is one of “particularly sensitive personal data” — they may therefore only be processed with an express legal basis and under strict security measures.
To ensure that exchanges remain secure and legally compliant in everyday practice, the following basic principles should be observed:
- Obtain consent: Patients must agree in advance that their data may be processed or transmitted electronically. This step can easily be added to the digital anamnesis be integrated with Nelly.
- Create transparency: Disclose which data is used for what purpose and stored for how long.
- Note earmarking: Use data only for medically necessary or organizational purposes.
- Implement data minimization: Only collect as much information as is required for treatment.
- Use secure communication channels: Use encrypted emails, certified patient portals, or GDPR-compliant messengers. Only use tools whose server is located in the EU and that offer an order processing contract. Nelly solutions meet these points.
- Ensuring access protection: Secure devices with passwords, two-factor authentication, and role rights.
- Train team: Conduct regular data protection training for all employees.
- Documenting processing: Record data accesses, changes and deletions in a comprehensible manner. This point is usually handled automatically by digital tools such as Nelly.
- Observe the right to information: Patients have the right to view their stored data at any time. It helps here if the majority of documents are available digitally and not in paper files — another argument for Nelly Praxisportal.
Which communication models can be transferred to patient communication?
Digital tools can simplify many processes, but what helps with interpersonal communication in the treatment room? Bid here Communication models valuable orientation. They make visible what happens between the lines, how misunderstandings arise and how respectful dialogue works. The following models are particularly easy to transfer to everyday practice.
Transmitter receiver model (Shannon & Weaver)
Communication is an exchange of information that can easily be affected by disruptions. This model promotes awareness of clear language, active inquiry and reinsurance (“Did you mean that? “).
four-ear model (Schulz von Thun)
Each message contains four levels: cause, self-revelation, relationship, and appeal. This model helps to identify emotional undertones and avoid misunderstandings in doctor-patient conversations.
Watzlawick's 5 axioms
“You can't not communicate” — posture, tone of voice and body language always have an effect. This model sensitizes to non-verbal signals and includes aspects such as relationships, communication medium and interactions.
LIMO principle
LIMO principle for praise, interest, lack and openness. It helps to respond to complaints in an appreciative and solution-oriented manner: First thanks for the advice, then genuine interest, identify the defect objectively and offer a joint solution.
Checklist for respectful patient communication
It takes a lot of experience and practical practice to truly internalize all communication models. Sabine Monka-Lammering, teacher of dental professionals, has summarized the most important points of interpersonal patient communication for us: Tips for communicating with patients. Here you can find the Key statements as a practical checklist:
1. Positive atmosphere right from the start
- Friendly welcome with direct contact and eye contact.
- All employees wear name tags.
- Sign openness and peace: no eye rolls, no negative gestures.
- Actively provide new patients with orientation (waiting area, processes, contacts).
2. Speak clearly and listen actively
- Avoid or explain technical terms, use simple language.
- Convey complex information in stages (“salami technique”) and check understanding.
- Consciously perceive non-verbal signals (gaze, posture, pauses).
3. Appear empathically and authentically
- Empathize with the patient. (“I understand that this is burdensome.”)
- Show appreciation and recognize stress. (“I'll take a moment for you right away.”)
- Express empathy also through posture, facial expressions and voice.
5. Communicate clearly, honestly and in a solution-oriented way
- Provide transparent information on appointments, waiting times and treatment steps.
- Address topics directly but sensitively
- Choose positive wording (instead of “This is not my area of responsibility”, better “I will forward your question directly to my colleague.)
4. Mastering difficult situations with sensitivity
- Prepare sensitive topics particularly well: Know the anamnesis, diagnoses and progress so far.
- Allow the patient's feelings and react empathically; respect retreat.
- Don't label difficult patients as “annoying”, but show understanding for dissatisfaction (“Thank you for bringing this up”).
- Set limits when threats or aggression occur.